Upper Endoscopy
What is upper endoscopy?
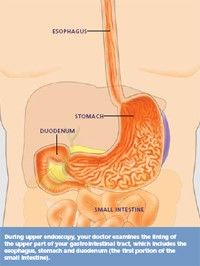
Upper endoscopy lets your doctor examine the lining of the upper part of your gastrointestinal tract, which includes the esophagus, stomach, and duodenum (the first portion of the small intestine). Your doctor will use a thin, flexible tube called an endoscope, which has its own lens and light source, and will view the images on a video monitor. You might hear your doctor or other medical staff refer to upper endoscopy as upper GI endoscopy, esophagogastroduodenoscopy (EGD), or panendoscopy. If you have specific questions about upper endoscopy, feel free to contact the experienced team at Northeastern Gastroenterology Associates.
Why is upper endoscopy done?
Upper endoscopy helps your doctor evaluate symptoms of persistent upper abdominal pain, nausea, vomiting, or difficulty swallowing. It's the best test for finding the cause of bleeding from the upper gastrointestinal tract. It's also more accurate than X-ray films for detecting inflammation, ulcers, and tumors of the esophagus, stomach, and duodenum.
Your doctor might use upper endoscopy to obtain a biopsy (small tissue samples). A biopsy helps your doctor distinguish between benign and malignant (cancerous) tissues. Remember, biopsies are taken for many reasons, and your doctor might order one even if he or she does not suspect cancer. For example, your doctor might use a biopsy to test for Helicobacter pylori, the bacterium that causes ulcers.
Your doctor might also use upper endoscopy to perform a cytology test, where he or she will introduce a small brush to collect cells for analysis.
Upper endoscopy is also used to treat conditions of the upper gastrointestinal tract. Your doctor can pass instruments through the endoscope to directly treat many abnormalities — this will cause you little or no discomfort. For example, your doctor might stretch (dilate) a narrowed area, remove polyps (usually benign growths) or treat bleeding.
What preparations are required?
An empty stomach allows for the best and safest examination, so you should have nothing to eat or drink, including water, after midnight prior to your scheduled procedure.
Tell your doctor in advance about any medications you take; you might need to adjust your usual dose for the examination. Discuss any allergies to medications as well as medical conditions, such as heart or lung disease.
Can I take my current medications?
Most medications can be continued as usual, but some medications can interfere with the preparation or the examination. Inform your doctor about medications you’re taking, particularly aspirin products or antiplatelet agents, arthritis medications, anticoagulants (blood thinners such as warfarin or heparin), clopidogrel, insulin, or iron products. Also, be sure to mention any allergies you have to medications.
What happens during upper endoscopy?
Your doctor might start by spraying your throat with a local anesthetic or by giving you a sedative to help you relax. You'll then lie on your side, and your doctor will pass the endoscope through your mouth and into the esophagus, stomach, and duodenum. The endoscope doesn't interfere with your breathing, most patients consider the test only slightly uncomfortable, and many patients fall asleep during the procedure.
What happens after upper endoscopy?
You will be monitored until most of the effects of the medication have worn off. Your throat might be a little sore, and you might feel bloated because of the air introduced into your stomach during the test. You will be able to eat after you leave unless your doctor instructs you otherwise.
Your physician will explain the results of the examination to you, although you'll probably have to wait for the results of any biopsies performed.
If you have been given sedatives during the procedure, someone must drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day.
What are the possible complications of upper endoscopy?
Although complications can occur, they are rare when doctors who are specially trained and experienced in this procedure perform the test. Bleeding can occur at a biopsy site or where a polyp was removed, but it's usually minimal and rarely requires follow-up. Perforation (a hole or tear in the gastrointestinal tract lining) may require surgery but this is a very uncommon complication. Some patients might have a reaction to the sedatives or complications from heart or lung disease.
Although complications after upper endoscopy are very uncommon, it's important to recognize early signs of possible complications. Contact your doctor immediately if you have a fever after the test or if you notice trouble swallowing or increasing throat, chest, or abdominal pain, or bleeding, including black stools. Note that bleeding can occur several days after the procedure.
If you have any concerns about a possible complication, it is always best to contact your doctor right away.
Since its founding in 1941, the American Society for Gastrointestinal Endoscopy (ASGE) has been dedicated to advancing patient care and digestive health by promoting excellence in gastrointestinal endoscopy. ASGE, with more than 11,000 members worldwide, promotes the highest standards for endoscopic training and practice, fosters endoscopic research, and is the foremost resource for endoscopic education.
This patient education was developed by the Publications Committee of the American Society for Gastrointestinal Endoscopy. This information is the opinion of and provided by the American Society for Gastrointestinal Endoscopy.
Copyright ©2010. American Society for Gastrointestinal Endoscopy. All rights reserved. This information may not be reproduced without express written permission by ASGE. For permission requests, please contact the ASGE Communications Department at 630-673-0600.
